Monday, February 04, 2008
Thursday, January 31, 2008
Monday, October 29, 2007
Friday, August 10, 2007
Friday, July 20, 2007
Quiz For Skin Station
Labels: Quiz series, Skin, Station 5
Sunday, June 17, 2007
Some Drills On Station 5 (Part 3)




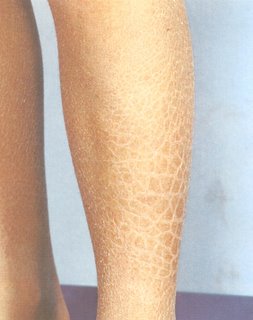
This series of photos belongs to a lady who presents with a rash.
The registrar in-charge in the PACES centre would be too happy to include cases like this in station 5, if they happen to land up in the ward at the right timing :)
State your diagnosis and the differential causes.
How would you manage this lady?
Labels: Quiz series, Skin, Station 5
Friday, March 16, 2007
Pustular Psoriasis



Stem
"This young man presented with this condition after being given some treatment for a his plaque psoriasis . Please examine his skin"
Suggested presentation
This febirle unwell-looking young man has generalised widespread creamy white pustules with an erythematous base. Some of the pustules have erupted, resulting in red oozing erosions . The palms and soles are also involved. He also has generalised onycholysis with discolouration and misshaped toes and fingernails.The patient has tenderness and warmth over both knee joints.
The diagnosis is pustular psoriasis complicated by gout. The likely cause for this presentation is massive intradermal steriod injection.
(Patient in this picture had pre-existing plaque psoriasis, so did his father and paternal grandfather. He was given Intradermal methylprednisolone 200mg daily instead of the recommended 10mg per month. Not shown inthe pictres, he had evidence of plaques on his elbows, hairlines and behind the ears)
Questions that may be asked
1. What differentiates this from skin infections?
The pustules are sterile on culture and the patient's white cell count may be normal
2. What is explanation for the patient's knee pain?
Psoriasis is a condition where there is increased cell turnover so there is hyperuricaemia, which results in crystal deposition in knee joins, giving rise to gout.
3, How would you manage this patient?
The patient should be managed like a exfoliative erythrodermic patient, paying close attention to barrier nursing, fluid replacement, prompt treatment of infections, adequate nutrition
4. Name me the definitive treatment for pustular psoriasis.
Acitretin, an oral retinoid.
Contributed by Giant Eagle
Wednesday, January 17, 2007
Some Drills On Station 5 (Part 1)
Let's ride!
Stem: Look at this patient's face and tell me what you think.
Suggested presentation:
This patient has herpes zoster ophthalmicus as evidenced by an area of confluent erythematous papules and vesicles, some of which are crusted. The area affected coincides with the region served by the ophthalmic branch of the trigeminal nerve and hence the diagnosis. I would end my examination by looking closely for any corneal involvement and preferably under a slit-lamp.
Q: What is the early sign would you look for in ophthalmic herpes?
A: I would look hard for the presence of Hutchinson's sign.
Q: Why would it be important to look for this sign?
A: Ophthalmic herpes could be sight-threatening if left untreated. Hutchinson's sign is one of the early signs of eye involvement.

A: A full 7-10 day course of oral acyclovir 800mg 5x/d. I would refer him to an ophthalmologist for full ophthalmological assessment.
Saturday, December 09, 2006
Skin: Hyperpigmentation


Possiblity of opening statments
Look this lady who presented with weakness, loss of appetite and weight loss.
Suggested examination method
Hands-look at palmar creases for hyperpigmentation (Compare with your own palm)
Mouth-look at tongue, buccal mucosa for hyperpigmentation
Elbow: pressure points hyperpigmentation
Other sites: nipples, previous scars
Look for vitiligo
Tell examiner you would like to complete examination by:
checking her blood pressure (postural hypotension)
look for sparse axillary and puvic hair
Abdomen-?scars of previous bilateral adrenalectomy
Ask to check for visual field defect if you suspect Nelson's Syndrome.
Remember Nelson's syndrome is a enlarging pituitary tumour caused by previous bilateral adrenalectomy (done in the past for treatment of Cushing's Disease. Hyperpigmentation caused by high ACTH levels.)
Suggested presentation
"This young lady has generalized hyperpigmentation, which is more marked in the tongue and the palmar creases. The history suggest that she has Addison's disease. "
Questions you may be asked
(1) What are the causes of Addison's disease?
Idiopathic (80%)
TB (important to remember if you are taking exam in Singapore/Malaysia)
Metastasis
HIV infection
(2) How will you investigate this patient?
Biochemical tests to look for hypoNa, hyperK, metabolic acidosis
Blood glucose to look for hypoglycemia
I will do a screening test using the synacthen test to confirm the diagnosis.
I will also measure ACTH levels and cortisol levels.
Suggested reading for this topic
Polyglandular syndrome type I and II
Interpreting the synacthen tests.
Contributed by Lee Jun @ Giant Eagle @ Suikotsu (Sleeping Bone)
References:
250 cases in clinical medicine by Baliga
An Aid to the MRCP PACES by Ryder
Monday, October 09, 2006
Lipodystrophy




Opening Statement
"This 17 year old girl presented to endocrine clinic with a history of polyuria and polydypsia. Please look at her and proceed."
This young girl who is short for her age has masculine facial appearance caused by loss of fat in the face. She has prominent muscles and inframazillary dimples.She also has loss of fat (fat atrophy) in the arms and hands, giving her a muscular appearance.
The diagnosis is partial lipodystrophy.
As the opening statement says she has polyuria and polydyspia, I would like to do a urine dipstick for sugar as this condition is associated with diabetes
Questions you may be asked
(1) What other conditions may be associated with lipodystrophy apart from diabetes
**HIV on antiretroviral therapy
**Mesangiocapillary glomerulonephritis
**Localized scleorderma
**Morphea
**Chronic replasing panniculitis
Contributed by Giant Eagle
Sunday, September 03, 2006
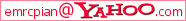
Some Pics Of Hansen's Disease
It is still not uncommon to see leprosy patient in Malaysia although we had achieved the WHO "elimination" level i.e. prevalence rate of less than 1 case per 10,000 inhabitants.
Here are some pictures of lepromatous leprosy patient from Sarawak. - courtesy of Giant Eagle.



Dermatomyositis
This lady has dermatomyositis. She has a heliotrope rash over the knuckles (GOTTRON"S Papules), back of the hands, eyelids and periorbital area. She also has nail fold telangiectasia.
(Look also in elbows and knees for Gottron's papules, it may be the only clue you have)
She also has Cushiongoid features, likely due to steroid treatment. (Mention other complications of steroid treatment if any-Cataract, vertebrae fracture, obesity).
There is also proximal muscle weakness and tenderness and the patient has had a muscle biopsy done (look for scars on thigh/upper arm)
Functionally, she has impaired swallowing as she requires a Nasogastric tube
NB Candidates often mispronouce "Gottron's" as "Grotton's". Be careful! Look for other things such as Raynauds, SLE
Questions that could be asked
1. How would you manage this patient?
**I would like to confirm my diagnosis of dermatomyositis by doing the appropriate investigations (eg muscle biopsy, Electromyelogram)
**As this lady is over 40, I would also investigate for underlying malignancy (mention NPC, breast, ovary, Lung and GIT) I would also investigate for connective tissue diseases.
**I will also start patient on high dose steroids and add on steroid sparing drugs.This patient also needs nutritional support as she is cachetic and has dysphagia caused by the disease.(Hopefully by the time you reach this station, your time is up)
2. How to differentiate this rash from SLE rash?**In SLE, the rash spares the knuckles, and involves the phalanges.
3. How would you classify polymyositis-dermatomyositi?
**I Primary idiopathic polymyositis
**II Primary idiopathic dermatomyositis
**III Dermatomyositis (Or polymyositis) with neoplasm
**IV Childhood dermatomyositis
**V polymyositis/dermatomyositis with collagen vascular disease
The above case and photos are contributed by Giant EagleWednesday, August 16, 2006
Hansen's Disease

What is your diagnosis if this case appear in skin substation? It is not JVP nor Corrigan's sign! It is a thicken great auricular nerve.
 Hypopigmented macules in confluence (patches) of tuberculoid leprosy.
Hypopigmented macules in confluence (patches) of tuberculoid leprosy.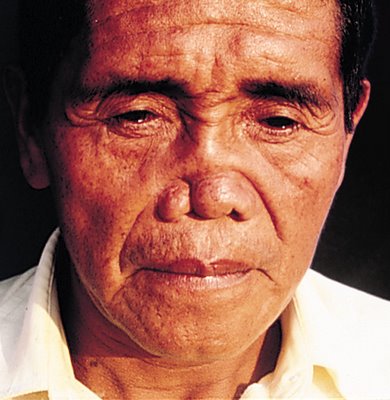 "Leonine facies" of diffuse lepromatous leprosy.
"Leonine facies" of diffuse lepromatous leprosy.
Wednesday, June 14, 2006
Spot diagnosis: Neurofibromatosis
One of the spot diagnosis in skin substation. As a PACES candidate, we need to demonstrate the various skin lesions (fibroma, plexiform neurofibroma, cafe-au-lait spots, axillary freckles) and also check for complications such as:
*Check hearing (acoustic neuroma)
*Visual acuity and fundi (optic glioma)
*Look for kyphoscoliosis
*Check BP for HPT in phaeochromocytoma



Monday, June 05, 2006
Basic Dermatology (2)
1. Vesicles and Bullae
** These terms describe different sizes of blister i.e. circumscribed elevation containing fluid.
** Vesicles(<5mm),>5mm)
** Examples: herpes simplex, pemphigus, pemphigoid.
2. Pustules
** A visible accumulation of free pus.
** Examples: pustular psoriasis, acne

3. Crust
** An accumulation of dried exudate, serum, blood. It is commonly known as scab.
** Examples: impetigo, ecthyma.

4. Scale
** Flaking of the skin surface due to increased loss from the stratum corneum(SC).
** It implies an abnormality in SC formation or damage to the epidermis.
** Examples: psoriasis, ichthyosis, tinea infections
5. Lichenification
** Areas of increased epidermal thickness secondary to chronic rubbing.
** Examples: eczema, lichen simplex chronicus

6. Atrophy
** Diminution of some or all layers of skin.
** In epidermal atrophy, the epidermis is thin, transparent and the vessels are prominent.
** Examples: Steroids induced atrophy

7. Excoriations
** A shallow abrasion due to scratching
** It is seen in itchy skin conditions like eczema, scabies, urticaria.

Able to give an accurate description of the skin lesions now?